Amid concerns about primary care provider shortages, especially in light of health reform coverage expansions in 2014, some believe that revising state laws governing nurse practitioners’ (NP) scope of practice is a way to increase primary care capacity. State laws vary widely in the level of physician oversight required for nurse practitioners, with some states allowing NPs to practice independently, while others limit NPs’ authority to diagnose, treat and prescribe medications to patients without supervision. In six states with a wide range of scope-of-practice laws—Arizona, Arkansas, Indiana, Maryland, Massachusetts and Michigan—the laws in and of themselves do not appear to restrict what services NPs can provide to patients, according to a new qualitative study by the Center for Studying Health System Change (HSC). However, scope-of-practice laws do appear to have a substantial indirect impact because requirements for physician supervision affect practice opportunities for NPs and may influence payer policies for nurse practitioners. Such policies include whether NPs are recognized as primary care providers and included by health plans in provider networks and whether NPs can bill and be paid directly. States with more restrictive scope-of-practice laws are associated with more challenging environments for NPs to bill public and private payers, order certain tests, and establish independent primary care practices. To ensure effective use of NPs in primary care settings, policy makers may want to consider regulatory changes beyond revising scope-of-practice laws, such as explicitly granting NPs authority as primary care providers under Medicaid or encouraging health plans to pay nurse practitioners directly.
- Scope of Practice and Nurse Practitioners
- Effect on Care Delivery
- Payer Policies Restrict NPs
- Policy Considerations
- Notes
- Data Source
Scope of Practice and Nurse Practitioners
With the United States facing a large and growing shortage of primary care practitioners, ensuring adequate access to care is a major policy concern.1 The problem is expected to worsen as the population continues to age and an estimated 30 million people gain access to health coverage, beginning in 2014, under the Patient Protection and Affordable Care Act of 2010.
One possible approach to alleviating pressures on the primary care workforce is greater use of nurse practitioners and physician assistants, which could both increase the number of primary care providers and potentially free up physicians to care for more complex patients. Nurse practitioners are registered nurses who have completed additional graduate-level education and trained to provide a broad range of primary care services (see box below for more about NP qualifications).
In contrast to NPs, physician assistants are trained to practice medicine under the supervision of a physician, and more than two-thirds work with specialist physicians.2 According to the American Academy of Nurse Practitioners, 89 percent of NPs are trained in primary care, and more than 75 percent practice in primary care settings. In 2010, an estimated 56,000 NPs practiced primary care in the United States, compared to approximately 209,000 physicians in primary care practice.3
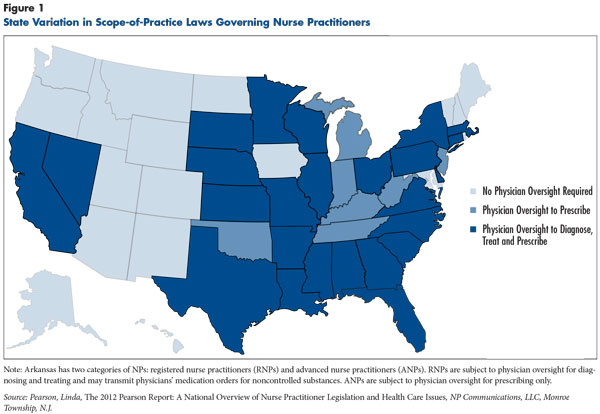
The clinical role of NPs is governed largely by state scope-of-practice (SOP) laws that determine the range of services NPs can provide and the extent to which they can practice independently. State SOP laws vary widely in the degree of autonomy granted NPs to treat and prescribe medications for patients without physician supervision or collaboration.4 Currently, 18 states plus the District of Columbia permit NPs to diagnose and treat patients and prescribe medications without physician oversight, while seven states require physician oversight of NP prescribing only, and 25 states require oversight of NPs’ diagnoses, treatment plans and prescribing 5 (see Figure 1).
A recent National Governors Association report recommended that states consider liberalizing state SOP laws to permit more autonomy in NP practice as one way to help meet the growing demand for primary care services.6 NPs may be an attractive solution to the primary care workforce shortage because they command lower salaries and can be trained more quickly and at lower cost than physicians. While NPs and physicians perform similarly on several process and outcome measures of care quality, NPs and physicians often strongly disagree about which professionals are qualified to perform what tasks.7 As a result, changing state scope-of-practice laws often is a highly contentious process.
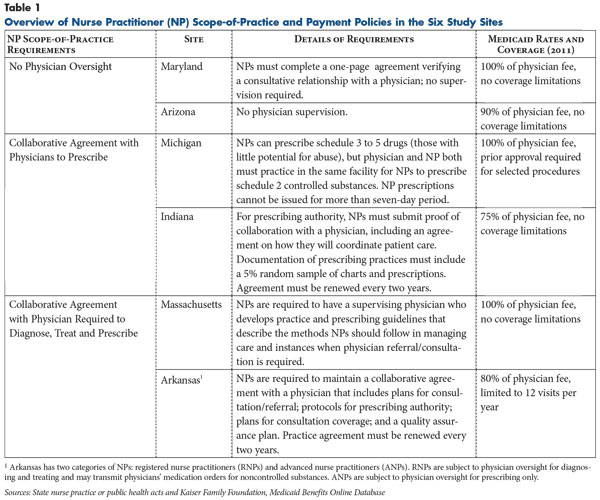
This Research Brief examines variations in SOP laws for NPs across six states—Arkansas, Arizona, Indiana, Maryland, Massachusetts and Michigan—to explore the extent to which these laws hinder efficient use of NPs in primary care settings, as well as facilitators and barriers to NP practice across communities (see Data Source). Scope-of-practice laws in the six states represent a range of restrictiveness, from Arizona allowing independent practice to Arkansas8 requiring direct physician supervision of NP diagnoses, treatment and prescribing (see Table 1).
Nurse Practitioner Qualifications
In the United States, nurse practitioners fall under the umbrella of advanced practice registered nurses, along with certified nurse midwives, clinical nurse specialists and certified nurse anesthetists. NPs are trained to diagnose and treat both physical and mental conditions through comprehensive history taking, physical exams, and ordering and interpretation of diagnostic tests. In contrast with physicians, NPs’ authority to diagnose, treat or prescribe varies depending on state, hospital and payer policies.
NPs are trained at the graduate level and generally have a master’s of nursing degree or a doctor of nursing practice degree, with a specialization in primary care, acute care or psychiatric/mental health nursing, sometimes with a focus on pediatrics, adult/gerontology or women’s health. NPs must qualify as a registered nurse before they can complete a graduate-level nurse practitioner program.
All NPs must pass a national board certification exam in their area of specialty to qualify for licensing in their state. Master’s-level training takes one to two years of full-time study and includes clinical rotations. Doctoral-trained NPs typically complete another year of post-master’s training and complete a higher level of clinical hours.
NPs are licensed in all states and the District of Columbia and practice under the rules and laws of the state in which they are licensed. State boards of nursing regulate nurse practitioners, and each state has its own licensing and certification criteria. In some states, state boards of nursing and medicine may jointly oversee NP licensing. In general, the criteria include completion of a graduate degree in nursing and board certification by an accrediting body, such as the American Nurses Credentialing Center or American Association of Colleges of Nursing.
Effect on Care Delivery
At the point of care, scope-of-practice laws were not found to have substantial impact across the study states on what services NPs can deliver, despite significant differences across states in the level of NP autonomy. Generally, NPs are trained to provide services similar to primary care physicians, though they do not complete a post-graduate residency training program and usually focus on chronic and preventive care management rather than complex diagnoses. Scope-of-practice laws generally do not spell out specific tasks that NPs can perform. Rather they authorize a broad range of practice and spell out whether or not physician supervision is required to carry out tasks.
Both primary care physician and NP respondents reported that within a practice the degree of supervision typically evolves over time and varies by NP and physician. Even in restrictive SOP states, most NPs described having latitude to make clinical decisions, although with a greater level of documented supervision. Moreover, they said working relationships with physician colleagues typically were more collaborative than supervisory in practice. Practice culture and individual practitioner traits, such as years at the organization or level of experience, seem to play an important role in determining everyday practice style and the level of autonomy NPs experience. One physician in Indiana, which limits NP prescribing authority, reflected a common sentiment, saying, “I have worked with and supervised many NPs, and for those that are just starting out, [chart review] is quite useful. For someone 20 years out? Not so much.”
Though SOP regulations do not necessarily limit the types of primary care services patients can receive from NPs, requirements for documented supervision do appear to impact where and how NPs can practice. Moreover, scope-of-practice laws can affect how NPs are used in care settings: NPs in states requiring physician oversight reported being more likely to have work delegated to them by physicians to satisfy supervision requirements. They also reported more often co-managing patient panels with physicians rather than acting as the sole, designated care provider. In practice, most respondents viewed collaborative agreements, which stipulate how the physician will supervise or monitor the nurse practitioner’s performance and competency, as a formality that does not stimulate meaningful interaction between NPs and physicians. However, these arrangements were reported to limit the range of practice settings for NPs, with notable impacts on underserved rural communities. For example, in Arkansas—one of the more restrictive states—an NP explained, “We are tethered to physicians; we can’t go farther out into rural communities than physicians are willing to go to provide care because of the collaborative practice agreement requirement. The collaborating physician has to be available and accessible, and I wouldn’t want to collaborate with someone 200 miles away.”
Scope-of-practice laws also may limit NPs to one site, which some respondents deemed a barrier because it prohibited them from working in multiple settings without separate agreements for each location. Maryland replaced a written collaborative agreement with a more streamlined process in 2010 requiring only a one-page form verifying that a consultation agreement is in place between an NP and physician for all practice locations. Practitioners noted no significant change to operations within existing practice settings, but NPs now can practice at any location rather than just the site of their collaborative agreement, expanding opportunities for them to deliver care. As a Maryland NP said, “[Removing the collaborative agreement] gives me a lot more freedom. For instance, I can cover an office in a neighboring county and do volunteer work in the community. Under the old agreement, I couldn’t have done that.”
State scope-of-practice laws also were reported to sometimes impede NPs’ efficiency. For example, in states that require oversight of prescribing authority—such as Arkansas and Michigan, which prohibit or restrict how NPs prescribe Schedule II controlled substances often used in treating pain—patients may encounter delays in securing prescriptions and refills. States also can exert some authority over hospital admitting privileges for NPs, though nearly all states defer to individual hospitals to set their own policies. Hospitals that only allow physicians to admit patients reportedly created challenges for patient follow up by an NP after discharge. As a practice manager of a multi-site primary care practice in Arkansas explained, “Patients have to be admitted under [the doctor’s] name. When the hospitalization records come back, they go to [the doctor], not to the NP. It puts them [the NPs] at a liability. We’ve ranted and raved about this issue with sending the records to the wrong person.”
Payer Policies Restrict NPs
Many NP respondents reported that payer policies had more of an impact than SOP laws on how and where they can practice. However, research has found that the level of restrictiveness in state scope-of-practice laws appears to be associated with the level of autonomy granted to NPs through public and private payer policies.9 Payers are in a position to determine what services NPs are paid for, their payment rates, whether NPs are designated as primary care providers and assigned their own patient panels, and whether NPs can be paid directly. Restrictive SOP laws, in conjunction with strict payer policies, reportedly limit NPs to working as employees of physician practices, hospitals or other entities rather than in their own independent practices. Given the interaction of payment and SOP policies, it’s unclear how more opportunities to practice independently would affect NP supply.
While both private and public payers typically must adhere to state SOP laws in their policies, payers often impose additional restrictions. For example, in Arkansas and Indiana, which do not allow autonomous practice, NPs are not recognized as primary care providers by traditional Medicaid, potentially constraining the reach of NPs’ services. Arkansas’ Medicaid program also will not pay for streptococcal screens or influenza swabs done by NPs. Notably, in both of these examples, the state’s SOP laws do not prohibit these activities by NPs, but also do not grant them explicitly, leaving these payment restrictions as longstanding Medicaid policies.
Commercial health plan payment policies for NPs vary considerably, and the relationship between these policies and SOP laws is often difficult to disentangle. It is fairly common for commercial health plans not to recognize NPs as primary care providers in plan networks; plans also can decline to credential or directly pay NPs for services. One respondent suggested that some payer policies may be a reaction to the extra administrative efforts involved in recognizing NPs as primary care providers, surmising that, “Part of a health plan’s resistance [is that] when you credential a whole bunch of providers, it is a lot of work.” Other respondents suggested that some payers may simply be reluctant to alter longstanding policies. (See box below for more about typical payer policies for NPs).
Given payer restrictions, many respondents reported that NP services are often provided as “incident-to” a physician’s services, a practice and billing arrangement that allows billing for NP care delivery under a physician’s name. The Centers for Medicare & Medicaid Services defines care as incidental if the care is provided under strict supervision criteria, including the physician being on site and the patient receiving care in accordance with the physician’s treatment plan.
The incident-to designation reportedly limits NP autonomy and minimizes the role of NPs as primary care providers. In states where NPs are not recognized as primary care providers in health plan networks, incident-to billing appeared to be more common. In these cases, NPs may provide a substantial amount of care but must be under a strict level of physician oversight. The payment for incident-to services provided by NPs at 100 percent of the physician rate has led some NPs to report pressure from physician employers against seeking direct payment as a designated primary care provider when it results in lower payment to the practice. Under this structure, NPs described being constrained in where and how they practice and further tethered to physicians geographically.
Medicare policies, which are uniform nationally, also affect the extent to which NPs are able to deliver care efficiently. For example, NPs are unable to order home health care or durable medical equipment for Medicare patients, regardless of whether they are designated as the sole primary care provider. Even in states that allow NPs to practice independently, such Medicare policies reportedly pose significant barriers to care delivery, making it difficult to practice without a collaborating physician. One respondent described the difficulties arising from these policies, saying, “I have to make a note, and then have to find a physician to sign it to certify that the patient still needs home care. The physician has never seen the patient, has no time to look up the information in that chart, so they totally rely on me [for my assessment of the patient]. And, I can’t tell you how often that note to the physician gets lost [and creates delays for the patient].”
Public and private payer policies also may preclude NPs from establishing their own primary care practices, even in states where scope-of-practice laws allow NPs complete autonomy. Lack of direct payment or low payment rates reportedly discourages many NPs from establishing or leading an independent practice, particularly given high overhead and costs associated with investments in electronic health records and other infrastructure. Even in states where health plans pay NPs directly, respondents noted that it can be difficult to maintain an adequate volume of patients that are covered by such plans and whose plans pay at a rate that keeps NP practices financially sustainable. A respondent explained that, “Arizona has had autonomous practices for 15 years, but it has not resulted in an increase in the number of NP-led practices, and it’s around being able to generate enough revenue to support the practice. So the scope-of-practice laws in the state and the reimbursement issues, you have got to have [solutions to address] both.”
Nurse Practitioner Payment Policies
A number of federal, state and payer-specific laws and policies govern payment for services rendered by a nurse practitioner. Most NPs maintain their own individual national provider identification (NPI) number, which is required for electronic transactions, including billing, referrals and prescribing.
To be listed as the rendering provider on an insurance claim, an NP must have an individual NPI number and be credentialed, or officially recognized for direct payment, by the payer. Some states mandate credentialing of NPs by third-party payers for all or a subset of services.10 Others may neither require nor prohibit insurer recognition of advanced practice registered nurses; however, research indicates that the default for third-party payers in these states is not to allow direct payment.11 If NPs can’t bill directly, the supervising physician’s NPI number reportedly is listed as the rendering provider and the service is reimbursed at the physician fee schedule amount.
For NPs able to bill directly as the rendering provider, payment levels can vary substantially. Medicare sets NP payment nationally at 85 percent of the physician fee schedule amount, while Medicaid fee-for-service payment is determined on a state-by-state basis, with roughly half of states providing pay parity with physicians, and others reimbursing between 75 percent and 95 percent of physician payment rates.12 Commercial health plans that pay for NP services, whether directly or to an employer, typically pay anywhere from 70 percent to 100 percent of the physician rate.13
Policy Considerations
Policy makers may wish to consider a variety of approaches to expand opportunities for NPs to deliver primary care services, particularly in areas where a shortage of providers is already documented or projected to worsen. Though the number of NPs is expected to almost double by 2025, laws that restrict how and where NPs may practice or be employed, including requirements for geographic proximity to a collaborating physician, limit the potential capacity of the NPs to meet increasing patient demand.14
In part to address these issues of professionalism and autonomy, the American Association of Colleges of Nursing (AACN) will raise accreditation standards for advanced nursing practice programs from a master’s degree to a doctoral degree in nursing practice (D.N.P.) starting in 2015, citing the need for NPs to develop more advanced competencies and prepare for greater leadership roles in the future. But, this measure may hamper the expected growth in NP supply since the additional training will take longer and cost more.15
There are two main approaches for policy makers to consider if they wish to alter the opportunities for NPs to have broader participation in the primary care workforce: state legislative reforms and public payer reforms.
State legislative reforms. Examining state scope-of-practice laws may be the first of many steps necessary to address how NPs may be best utilized. Some states—Massachusetts and Michigan, for example—have considered or passed legislation to expand the role of nurse practitioners in delivering primary care services.16 Massachusetts experienced shortages of primary care providers available to newly insured persons after implementing near-universal health coverage in 2006 and recently expanded the role of NPs in primary care settings by changing the legal definition of a primary care provider. Michigan lawmakers, citing an inadequate supply of practitioners in many counties, also have introduced legislation to expand NPs’ scope of practice for prescribing authority and to recognize NPs separately from registered nurses.
Several states also maintain laws and regulations outside of SOP laws that restrict the use of NPs in primary care settings and that may merit re-evaluation. For example, in Michigan, only members of “learned professions”—such as dentists, physicians and attorneys—may form a professional limited liability company or a professional services corporation. This forces NPs to either practice under the business license of a physician or hire a physician collaborator to operate their own practice; few NPs pursue this path. Another example is Indiana, where state law authorizing clinicians to order physical therapy was written before the field of advanced practice nursing existed, and the law has not been updated to include NPs.
How states move forward may affect the ability of NPs to participate in efforts established under health reform to incentivize better integration and coordination of services in primary care settings. NP respondents are concerned that, although they may handle many of the coordination aspects of care promoted by care delivery models and payment arrangements under reform, they might be excluded from payment reforms that fall under state discretion. For example, the Medicare Accountable Care Organization (ACO) Shared Savings Program allows NPs to participate as providers if they are partnered with or employed by a hospital participating in an ACO. However, the extent to which NPs participate in ACOs will be determined in large part by state scope-of-practice laws.
Public payer reforms. Public payer reforms may contribute to addressing primary care workforce shortages for people covered by Medicare, Medicaid and other public programs. For example, exceptions to state SOP laws have long existed for Medicare-certified Rural Health Clinics (RHCs), which are located in medically underserved areas. In RHCs, NPs are recognized as primary care providers, operate with an expanded scope of practice and are paid the same rate as physicians.17 Provider shortages in these areas precipitated these policies, and it is possible that these types of measures may become more common as millions of people gain health coverage under health reform and provider shortages worsen.
Revising state regulation of Medicaid managed care plans, which cover most Medicaid enrollees, may be a more immediate and politically feasible way to expand effective utilization of NPs in primary care. Currently, one-third of states do not explicitly allow NPs to be designated as primary care providers in Medicaid managed care networks. While NPs can treat Medicaid patients as part of a care team, inability to maintain their own patient panels may limit their capacity to serve more patients. Even in states where NPs are recognized as primary care providers, managed care plan rates often mirror traditional Medicaid rates set by the state and vary substantially. State policies mandating recognition of NPs as primary care providers in managed care networks and raising the reimbursement rates on NP-provided services within their scope of training could encourage broader and more efficient use of NPs in primary care settings.
Some evidence suggests that Medicaid efforts to reduce limitations on NPs’ autonomy may encourage other payers and providers to amend their policies and practices. One NP respondent reported, “We got a rule in statute under Medicaid [that allowed NPs to be recognized as primary care providers (PCPs)], and once we did that, we were able to do that with other insurance companies…we said we are designated as PCPs in the state. That sort of enabled the commercial payers to make that decision to move things around.”
Clarification: On March 1, 2013, this Research Brief was updated to make clear that Arkansas has two categories of nurse practitioners with different physician supervision requirements. All online documents reflect this update.
Notes
1. Carrier, Emily, Tracy Yee and Lucy Stark, Matching Supply to Demand: Addressing the U.S. Primary Care Workforce Shortage, Policy Analysis No. 7, National Institute for Health Care Reform, Washington, D.C. (December 2011).
2. American Academy of Physician Assistants (AAPA), 2010 AAPA Physician Assistant Census, Alexandria, Va. (2011).
3. U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality, Primary Care Workforce Facts and Stats: Overview, Rockville, Md. (January 2012).
4. National Conference of State Legislatures, Scope of Practice Legislative Database, http://www.ncsl.org/issues-research/health/scope-of-practice-legislation-tracking-database.aspx (accessed on Feb. 12, 2013).
5. Pearson, Linda, The 2012 Pearson Report: A National Overview of Nurse Practitioner Legislation and Health Care Issues, NP Communications, LLC, Monroe Township, N.J.
6. National Governors Association, The Role of Nurse Practitioners in Meeting Increasing Demand for Primary Care, Washington, D.C. (Dec. 20, 2012).
7. Krupa, Carolyne, “Larger Role Sought for Advanced Practice Nurses,” American Medical News, (Jan. 13, 2012); Newhouse, Robin P., et al., “Advanced Practice Nurse Outcomes 1990-2008: A Systematic Review,” Nursing Economics, Vol. 29, No. 5 (October 2011); and Naylor, Mary D., and Ellen T. Kurtzman, “The Role Of Nurse Practitioners In Reinventing Primary Care,” Health Affairs, Vol. 29, No. 5 (May 2010).
8. Arkansas has two categories of NPs: registered nurse practitioners (RNPs) and advanced nurse practitioners (ANPs). RNPs are subject to physician oversight for diagnosing and treating and may transmit physicians’ medication orders for noncontrolled substances. ANPs are subject to physician oversight for prescribing only.
9. Hansen-Turton, Tine, et al., “Insurers’ Contracting Policies on Nurse Practitioners as Primary Care Providers: The Current Landscape and What Needs to Change,” Policy, Politics and Nursing Practice, Vol. 7, No. 3 (August 2006).
10. National Conference of State Legislatures (2012).
11. Pearson, Linda, The 2009 Pearson Report: A National Overview of Nurse Practitioner Legislation and Health Care Issues, NP Communications, LLC, Monroe Township, N.J.
12. The Kaiser Family Foundation, Medicaid Benefits: Online Database, http://medicaidbenefits.kff.org (accessed on Feb. 12, 2013).
13. National Conference of State Legislatures (2012).
14. Auerbach, David I., “Will the NP Workforce Grow in the Future? New Forecasts and Implications for Healthcare Delivery,” Medical Care, Vol. 50, No. 7 (July 2012).
15. Bellini, Sandra, and Regina M. Cusson, “The Doctor of Nursing Practice for Entry into Advanced Practice: The Controversy Continues as 2015 Looms,” Newborn and Infant Nursing Reviews, Vol. 12, No. 1 (March 2012).
16. Massachusetts General Law at http://www.malegislature.gov/Laws/GeneralLaws/PartI/TitleXXII/Chapter176R/Section3; and Michigan House Bill 4774 at http://legislature.mi.gov/doc.aspx?2011-HB-4774 (2011).
17. American Medical Association (AMA), AMA Scope of Practice Data Series: Nurse Practitioners, Chicago, Ill. (October 2009).
Data Source
This study examined the impact of state scope-of-practice laws and other market and organizational factors impacting the roles of nurse practitioners in primary care settings. Six states—Maryland, Arizona, Michigan, Indiana, Massachusetts and Arkansas—were selected to capture variation in levels of scope-of-practice requirements and to include states with recent or pending legislative changes affecting NPs. Thirty telephone interviews were conducted with nurse practitioners in primary care, multi-specialty, retail and occupational health settings and with practice managers and physicians working in settings that employ NPs. Interviews were conducted by two-person research teams between February and August 2012, and notes were transcribed and jointly reviewed for quality and validation purposes.